Did you know that the human body technically already has the tools needed to fight cancer?
Immunotherapy is a type of cancer treatment that uses the patient’s immune system to fight the cancer. When effectively conducted it can lead to long-term survival of the cancer patient. Cancer immunotherapy is driven by the body’s ability to have immune responses driven by tumour cell antigen-specific, T lymphocytes, that recognize and degrade tumour cells. The main reason why a cancer patient’s T cells can’t typically destroy these tumour cells is due to the immunosuppressive microenvironment that tumours form around themselves by suppressing their antigen expression. Cancer cells also take advantage of immune checkpoints in the body that are intended to hinder serious immune responses to avoid detection. However, this new study seems to have come up with a new form of ICB cancer immunotherapy that can effectively counter cancer cell deception tactics.
Immune checkpoint blockade (ICB) is a type of immunotherapy that is currently used to bypass this system to allow T cells more opportunities to destroy cancer cells. Type 1 conventional dendritic cells (cDC1s) are also important for ICB therapy since they have vital functions in the recruitment and activation of T cells. Researchers discovered that it is possible to effectively reprogram tumour cells using specific transcription factors to resemble cDC1s while remaining in the tumour’s microenvironment to teach the immune system to have an immune response when it sees these tumour cells
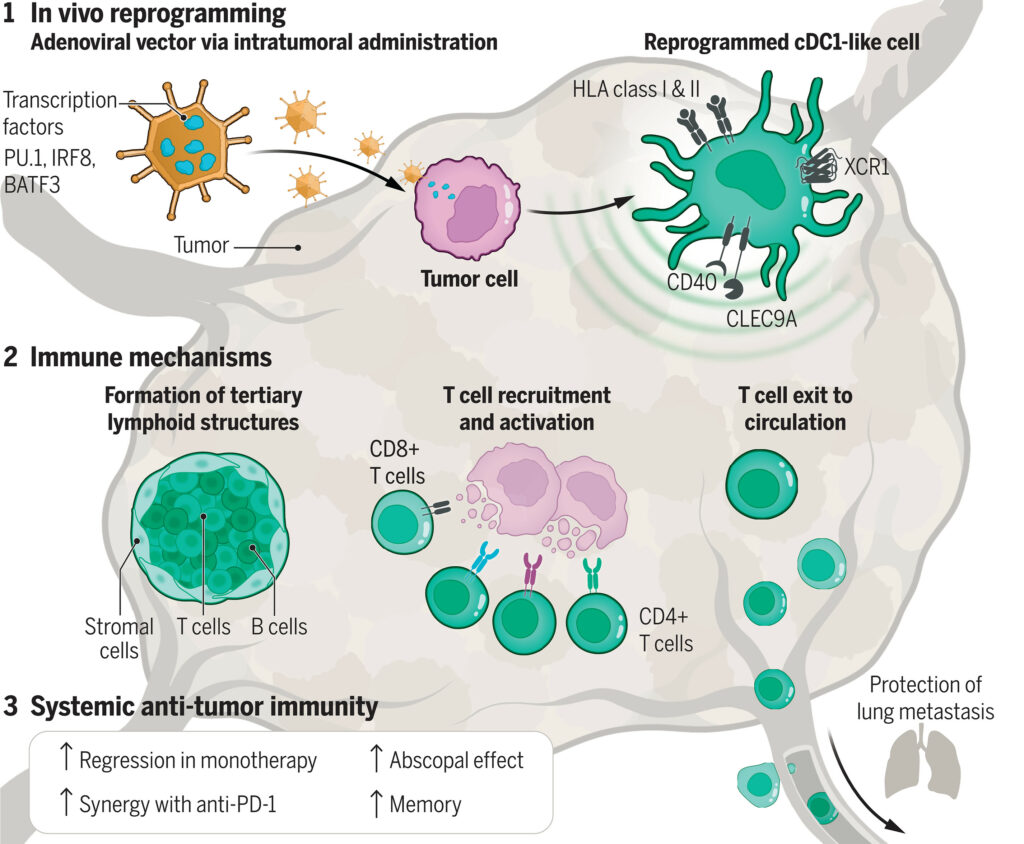
By delivering transcription factors PU.1, IRF8, and BATF3 (PIB) the researchers were able to enable tumour cells to resemble cDC1s and present specific antigens. They specifically chose PIB which had been shown to directly reprogram tumour cells into antigen-presenting cDC1-like cells in vitro within 9 days, according to past studies.
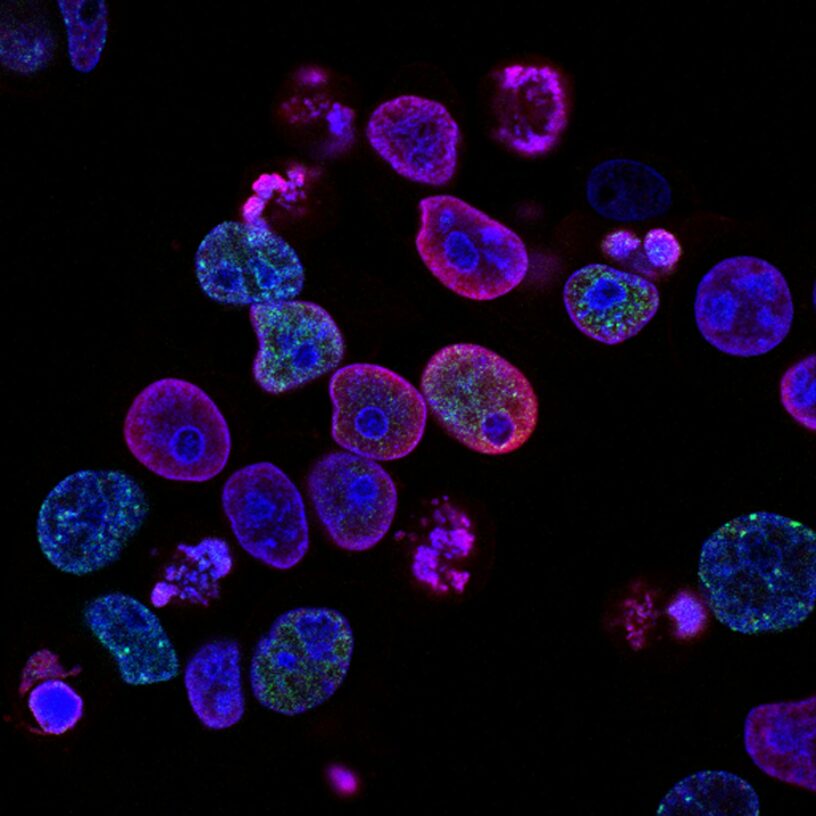
This research team prepared cultures of tumours as well as cells that had been modified to contain PIB using a method called transduction to see if they would be able to successfully reprogram them. When these mixtures had been incubated they had found that cDC1-like cells within tumours had formed and remodelled the tumour microenvironment. This caused the recruitment of T cells as well as other immune response reactions that led to cell regression.
What’s most impressive about this study was that they were able to achieve their desired results both in-vitro and in-vivo which can now be used as a preclinical proof-of-concept for a future tumour-specific immunotherapy. While there are certainly more steps to be taken to determine how to administer these therapies to humans in a clinical situation, this modified ICB therapy is certainly a game changer in cancer immunotherapy.
—
Adapted from: https://www.science.org/doi/10.1126/science.adn9083