Each year, cardiovascular diseases take the lives of 17.9 million people globally, with the majority of these deaths being a result of heart attacks. What happens immediately after a heart attack, or a myocardial infarction (MI), can determine one’s heart health for the rest of their life. But what if we could heal heart tissue faster and better than ever before, and reduce irreversible cardiac damage?
Previously, significant progress had been made in reducing MI death rates, yet there was lacking knowledge on the prevention and healing of cardiac tissue injuries post-MI. Realizing this, researchers at the School of Chemical and Biological Engineering at Seoul National University made a recent breakthrough in nanotechnology that offers hope to millions affected by heart attacks by developing a nanoparticle that chemically influences the role of neutrophils in the heart, and promotes tissue repair.
What are neutrophils and what do they have to do with the heart?
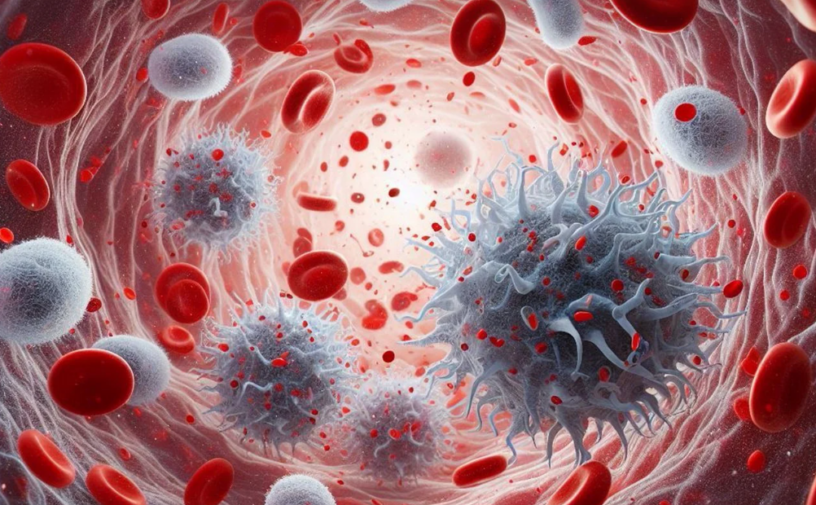
Neutrophils are a type of white blood cell that plays a prominent role in the immune system, including the production and reduction of inflammation in the heart after an MI via signaling pathways. Damage-associated molecular patterns (DAMPs) in the heart signal neutrophils to travel to the site of damage following an MI, which then proceed to be activated by reactive oxygen species-dependent (ROS) pathways. The activated neutrophils can then secrete a series of molecules, such as proteases and cytokines, which lead to further damage in cardiac cells and increase inflammation.
Following this, the neutrophils undergo NETosis, which is the main form of neutrophil death under inflammatory conditions. With the death of neutrophils, less cytokines and proteases are released, causing macrophages to polarize after sensing this decrease in molecule concentration. Similarly, macrophages polarize when they recognize the debris of dead neutrophils. Macrophages are another type of immune cell that are polarizable, meaning that they perform different functions depending on the environmental signals received. Once the heart is further inflamed, polarization switches them from a pro-inflammatory role to a healing one, jumpstarting the cardiac tissue recovery process.
The problem
While this may seem like an effective pathway to promote heart healing, researchers identified a harmful problem within this mechanism: the overexpression of neutrophil activation triggers the death of cardiac cells, resulting in potentially irreversible cardiac tissue damage post-MI. When the neutrophils get activated, the release of cytokines, proteases, and other molecules induce apoptosis, or cell death, of cardiac cells. With this knowledge, researchers realized that neutrophil activity must be reduced in order to prevent these damaging effects and mediate inflammation.
The solution
Researchers created roscovitine- and catalase-loaded poly(lactic-co-glycolic acid) nanoparticles (RC NPs) that regulate cardiac neutrophil lifespans by inducing targeted cell death, or apoptosis. These nanoparticles are tiny packages containing the drug roscovitine and a catalase. Think of RC NPs as hitchhikers: when they are injected into the blood (the highway of the body), they are picked up by neutrophils that are on their way to the post-MI heart. Once they reach the heart and the neutrophils are activated by ROS-dependent pathways, hydrogen peroxide is produced, which the catalase inside the nanoparticle can then turn into oxygen. The buildup of oxygen gas in the nanoparticle results in the rupture of the RC NPs, releasing the roscovitine drug.
Roscovitine is a type of inhibitor that is used to induce neutrophil apoptosis. With roscovitine, neutrophils can experience cell death specifically at the site of the infarcted heart at an earlier stage. This allows neutrophils to skip the line in the cardiac healing pathway, going straight to macrophage polarization without the release of cytokines and proteases or the enhancement of inflammation.
How was it done?
Extensive experimentation was done in order to develop the RC NPs. To start, researchers first had to determine if the movement of neutrophils from the bloodstream to the heart was uninterrupted by the RC NPs using a method called transwell migration assaying. In the lab, an environment that mimicked that of the body was created to test neutrophil movement in the presence of RC NPs and in the absence of RC NPs. On the transwell, the movement of RC NP positive neutrophils paralleled that of the control, showing that RC NPs did not influence neutrophil migration and were compatible with surrounding tissue.
Researchers then had to better understand the role of RC NPs on macrophage polarization. A coculture assay is a lab technique where two types of cells are grown together in the same environment to observe how they influence each other, and was used to observe macrophages and neutrophils. A coculture of macrophages and RC NP-absent neutrophils was compared against a coculture of macrophages and RC NP-present neutrophils. Analysis techniques were used to determine that macrophage polarization was much higher when grown in an environment with RC NP positive neutrophils compared to in an environment with neutrophils that lacked RC NPs, confirming that RC NPs effectively promote heart healing.
From previous scientific knowledge, researchers realized that after injection, RC NPs could be uptaken by two possible molecules: neutrophils or monocytes. To test which molecule predominated in nanoparticle uptake, researchers utilized a mouse model. Researchers injected RC NPs into mice and analyzed the circulation of the nanoparticles in monocytes or in neutrophils at different times. Using an analysis technique called flow cytometry, it was determined that at the early stages after injection of the nanoparticles, the majority of RC NPs were uptaken by neutrophils. This was a beneficial conclusion for the researchers as neutrophils are what needed to be targeted for this heart healing pathway.
Now what?
While nanotechnology may sound like science fiction, in reality it is opening the doors to a new era in heart health. RC NPs create a balance between allowing cardiac neutrophils to trigger signal transduction pathways to stimulate macrophage polarization, but induce their apoptosis before over-inflammation and cardiac damage is created. Though still in trial, RC NPs could one day revolutionize patient care by making heart attack recovery faster and more effective than ever.
Reference:
Kim, C., Kim, H., Sim, WS. et al. Spatiotemporal control of neutrophil fate to tune inflammation and repair for myocardial infarction therapy. Nat Commun 15, 8481 (2024). https://doi.org/10.1038/s41467-024-52812-6
Featured Image: https://pixabay.com/illustrations/wbc-leukocytes-antibodies-rbc-8791149/