In Vitro Fertilization has opened the doors to parenthood for millions of couples with fertility issues. According to International Committee for Monitoring Assisted Reproductive Technologies, 13 million babies to date have been conceived from IVF, with roughly five hundred thousand more born each year. Unfortunately, this figure still falls short of the number of couples attempting IVF. While IVF helps overcome barriers to fertilization, it cannot address a subsequent challenge: embryo health, a factor that ultimately determines the success of a pregnancy. More than half of aspiring parents undergoing treatment still fail to conceive or maintain healthy pregnancies due to the limited knowledge on the physiological conditions of their own bodies.
Developing technologies have directed researchers towards embryo treatment for the answer, and one method stands out: Intra-ovarian platelet-rich plasma injections. This treatment seeks to improve egg cell health prior to fertilization by supplementing nutrients from the mother’s blood. A recent studies on the treatment, published in the scientific journal Nature, investigated this proposal and found promising results for the treatment, based on an experiment conducted on 74 patients. Researchers from the Lee Women’s Hospital in Taiwan found that intra-ovarian platelet-rich plasma injections pre-fertilization have had positive post-fertilization effects on the quality of blastocysts.
Intra-ovarian Platelet-rich Plasma (PRP) Injections for Patient prior to Ovulation
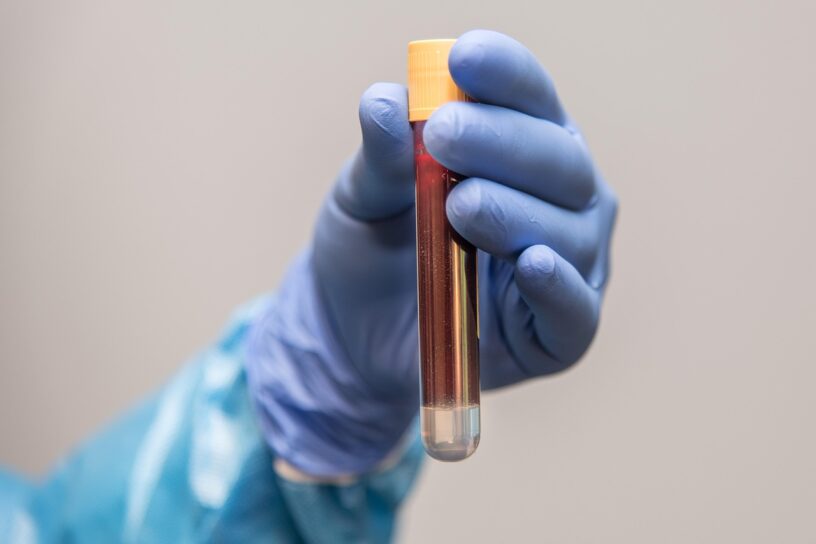
Blood flow is a crucial, arguably symbolic, process that fuels life. Blood is composed of red blood cells, whose primary role is oxygen delivery, and plasma, which is the solvent in which platelets, thousands of nutrient and protein types are delivered to individual cells. Utilizing this nutrient-dense solvent, researchers designed PRP injections extracted from blood plasma to supply to the ovary. This organ carry oocytes, which eventually mature into egg cells, female gametes that participate in fertilization.
Platelet-rich plasma is highly rejuvenating due to its diverse composition:
- Proteins, which can serve as clotting factors, or stimulate intracellular metabolic processes and intercellular communication processes.
- Cytokines, which are immune proteins that allow chemical signaling between the immune system and other cells.
- White blood cells that enhance immune response, and platelets, which are cell fragments that contain many cytoplasmic proteins and promote clotting at wound sites.
- Growth factors and hormones that can stimulate cell proliferation and maturation.

(Source image: Florida Joint Care Institute)
PRP injections make a potent wound-healing treatment that is widely used in surgery in orthopedics and obstetrics and gynecology to treat sexual or pelvic floor disorders. This use suggested that PRP injections in ovaries may promote the health and growth of oocytes to subsequently promote embryo health, which is the basis of this study. The treatment, derived from the patient’s own blood, is relatively low-risk in autoimmune complications. Of the 74 patients in the experiment, PRP injections were done on 44 patients at their follicular phase in the ovarian cycle, when follicles are growing and the endometrium walls thicken. This allows the oocytes to receive platelet-rich plasma before it matures in the ovulation phase. The remaining 30 patients do not have any treatment done, serving as the control group.
Evaluation of Blastocyst Quality after PRP Injections
Researchers induced ovulation using controlled ovarian hyperstimulation (COH). This technique is commonly used in IVF to induce multiple oocyte maturation using human hormones with the aim of obtaining a larger yield of egg cells to participate in fertilization in females. Progestin, the synthetic version of the female reproductive hormone progesterone, is used to stimulate ovulation to receive more egg cells.
A COH cycle was also done for all patients prior to treatment, and confirmed the quantity and quality of blastocysts were similar in all patients. The procedure was performed again in the immediate cycle for the control group, and after the injection treatment for the PRP group. COH was done typically during the ovulation phase of the patient’s ovarian cycle following the follicular phase, allowing researchers to obtain oocytes that had received PRP injections. After oocyte retrieval, eggs were fertilized with the sperm, resulting in an embryo which was grown into blastocysts in an in vitro medium.
Improvement of blastocyst quality
After the PRP group had received their injection, the average rate of total blastocysts had more than doubled in the PRP group, while the rate of good quality blastocyst increased from an average of 1% in the control group to 14% in the PRP group. The significant increase in total blastocysts and good quality blastocysts answered their hypothesis with a positive outcome: Intra-ovarian PRP injection induced a notable improvement in the quantity and quality of blastocysts.
The PRP group also had more blastocysts available to be analyzed through preimplantation genetic testing for aneuploidy (PGT-A), a diagnostic test to find if the embryonic cells have the correct number of chromosomes (euploidy), if it is irregularly numbered (aneuploidy) or if it is mixed with euploid and aneuploid cells (mosaic). Down syndrome is an example of aneuploidy. In the control group, only two patients out of 30 had one blastocyst available for PGT-A, and only one of which was euploid but resulted in a miscarriage. The PRP group, in contrast, had 22 patients with available blastocysts to analyze, which resulted in a 17.6% euploidy rate and 20.6% mosaic rate.
Researchers theorized that the diverse composition of growth factors and hormones may have enhanced embryo quality. This nutrient-rich blood can stimulate more oocytes to undergo second meiosis and mature to more viable egg cells. These egg cells have better health due the supply of nutrients and immunity from PRP injections, allowing for better growth of the embryo into blastocysts.
Potential in Assisted Reproductive Technology
IVF has gone a long way in enabling the dream of children for many families, and intra-ovarian PRP injections continue to extend the potential of assisted reproductive technology (ART). Couple may be able to better prepare their gametes prior to fertilization and allow higher chance of pregnancy with PRP injection treatment. While the study experimented on female patients, the treatment has to potential to be adapted to male patients, who have continued generation of gametes far into adulthood, and are likely more responsive to the technique. Another potential of intra-ovarian PRP therapy is reducing likelihood of aneuploidy, allowing mothers to carry healthier babies. While the technique is still being further tested and may not be exhaustive, it will undoubtedly be in high demand as an ART. Perhaps babies need milk even before they are born. PRP may be the maternal milk that embryos need to survive.
References
Adamson, G. D., Creighton, P., de Mouzon, J., Zegers-Hochschild, F., Dyer, S., & Chambers, G. M. (2025). How many infants have been born with the help of assisted reproductive technology? Fertility and Sterility, 124(1), 40–50. https://doi.org/10.1016/j.fertnstert.2025.02.009
Yu, TN., Chen, MJ., Lee, TH. et al. Intraovarian platelet-rich plasma injection significantly improves blastocyst yield and quality in IVF patients. Sci Rep 15, 1301 (2025). https://doi.org/10.1038/s41598-024-82630-1
Source image: https://pixabay.com/photos/blood-sample-test-tube-covid-test-6200015